Abstract

Primary central nervous system lymphoma (PCNSL) is a rare topographic variant of diffuse large B-cell lymphoma (DLBCL). First-line therapy is based on high-dose methotrexate. Post-induction treatment is recommended in chemotherapy-sensitive patients, but its modalities are matter of debate. While specific prognosis scales are useful in clinical trials, no dynamic prognostic marker is available to consider risk-adapted therapeutic strategies. We report here the prognostic value of early metabolic response by 18F-FDG PET/CT scanner (PET) in 27 newly diagnosed immunocompetent PCNSL patients.
Methods: Our patients were treated frontline by 375mg/m² Rituximab and 8g/m² Methotrexate at day 1 and 14, and Temozolomide 150mg/m² days 7 through 11, repeated for four cycles every four weeks (the RMT regimen). Whenever possible they received consolidation therapy by etoposide 40mg/kg on a continuous 96h infusion and cytarabine 2g/m² twice a day during 4 days (the EA regimen), or radiotherapy. Initial PET excluded a systemic localization of lymphoma in all patients. Response to treatment was evaluated according to international PCNSL collaborative group (IPCG) criteria. Brain magnetic resonance imaging (MRI) and PET were performed at diagnosis before any chemotherapy, after two and four cycles of RMT, and after treatment completion.
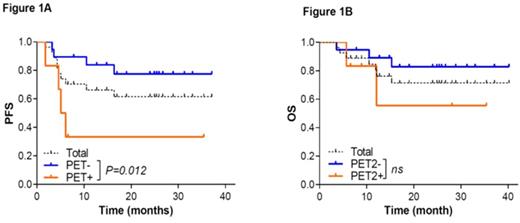
Results: Median age was 68. One patient had concomitant ocular involvement at diagnosis. Twenty patients (74%) completed the 4 cycles of RMT. Among the 7 remaining patients, causes of treatment discontinuation were lymphoma-unrelated death (n=2) and progression (n=5). Then 17 patients underwent a consolidation therapy, by EA in 13 patients, and by radiotherapy in 4 (23.4 Gy, n=3 and 30.4 Gy, n=1). Two patients had a watchful waiting strategy. Median follow-up was 25.4 month (6.1-40.2 month). After two cycles of RMT, 11 (40.7%) patients had a complete response or complete response unconfirmed (CR/CRu), 7 (25.9%) had a partial response (PR), 1 (3.7%) had a progressive disease (PD), 2 (7.4%) had a stable disease (SD) and 5 (18.5%) were not evaluated (NE) due to lymphoma-unrelated death in one and protocol deviation in four. After treatment completion, 19 (70.3%) patients were in CR and 6 (22.3%) had a PD. Two (7.4%) patients were NE due to lymphoma-unrelated death. Positive PET was defined by a new brain lesion or the persistence of 18F-FDG uptake compared to the controlateral parenchyma. Twenty five patients underwent PET after 2 cycle of RMT (PET2). Six (24%) had a positive PET2 (PET2+), and concomitant MRI showed CRu (n=1), PR (n=2), SD (n=2) and PD (n=1). Nineteen patients (76%) had a negative PET2 (PET2-), among whom we observed 10 CR/CRu, 5 PR and 4 NE by MRI. After treatment completion, 4 PET2+ patients (66%) had progressive disease. Only one patient with negative PET2- had a localized intraocular evolution with persistent MRI CR during induction therapy, and one patient in CR died from disease-unrelated cause. Predictive positive and negative values (PPV/PNV) of PET2 on end-of-treatment CR were 66.67% and 94.44%, respectively. During follow-up, one PET2- patient relapsed and another progressed to a fatal lymphoma-related ventriculitis. All SD/PD patients had hypermetabolic lesions, including at relapse. We observed a significant association between PET2 and end-of-therapy response (p=0.0004) and progression free survival (PFS, p=0.0378), while having no significant impact on overall survival (OS, p=0.3699). Two years PFS was 77% (CI 95% 50-91%) and 33% (CI 95% 50-67%) for PET2- and PET2+ patients, respectively (Figure 1). However, PET2 did not retain a significant prognostic value on PFS or OS in multivariate analysis.
Conclusion: We assessed for the first time the prognostic value of PET2 in a retrospective series of 27 newly diagnosed immunocompetent PCNSL patients homogeneously treated by the RMT regimen, and observed that PET2 correlated to MRI-assessed response and to PFS. PET2 negativity predicted a favorable outcome in all but one case (ocular relapse), suggesting that early metabolic response may identify chemosensitive patients, as demonstrated in systemic lymphoma. Future PCNSL clinical trials might therefore integrate PET in risk-stratified therapeutic strategies.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal